Abstract
Introduction: Serologic testing of post-transfusion reaction specimens aims to ascertain potentially accountable immune hemolytic incompatibility. With the exception of low-risk fevers or uncomplicated allergic reactions (ie- reactions with a likelihood of incompatibility that is deemed too low to justify testing), all transfusion reactions undergo serologic investigation as a matter of local institutional policy. However, compliance with guidelines, and the yields of testing according to reaction types, remain unknown. These measures may indicate the quality of applied practice, and provide evidence for maintaining (or changing) investigation algorithms.
Study Design and Methods: Interrogation of two hemovigilance databases identified all possible-to-definite transfusion reactions over a 4-year period (2013-2016) at four academic hospitals (with 1493 adult-care beds). The performance and outcome of reaction-oriented serology were assessed by site, year, reaction type, implicated product, and patient location. Serologic testing of transfusion reaction samples entailed the performance (and pre-transfusion comparison) of grouping (ABO, RHD type) and red cell antibody screening (indirect antiglobulin testing [IAT]), with a post-transfusion Coomb's/direct antiglobulin test [DAT]. Appropriate reflex tests (elutions, panel investigations, or IAT re-crossmatching) proceeded from pertinent positives. Allergic reactions were "complicated" if significant vital sign changes occurred, while fevers were "high-risk" (HRF) if symptomatic or if the Tmax rose to ≥39⁰C. Cardiorespiratory reactions (CRR) involved symptomatic and/or objective disturbances in heart/lung function, while unclassifiable presentations (changes in sensorium or non-precordial pain) were placed in an atypical/"other" category for analysis.
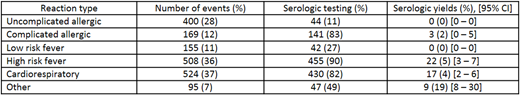
Results: Sites received 338-367 reaction referrals per year. By referral proportions (and with overlaps), fevers accounted for 47% of events, allergic disturbances for 40%, and CRR events for 37%, with unclassifiable reactions in 7% (Table). Serologic examination occurred in 773 (55%) of 1412 referrals (of which 1346 were deemed to be transfusion-attributable disturbances, among 1119 unique recipients). The majority of cases (1153 or 82%) were compliant with guidelines. Similar proportions deviated to over-testing (85/550 [15%]) as to under-testing (174/862 [20%]). Overall, 34 (4.4%) of 773 cases yielded a new finding, with 6 (0.8%) reflecting (new or recrudescent) host-derived anti-erythrocyte antibodies, for a number-needed-to-test (NNT) of 129. Serologic yields occurred in all categories where testing was mandated, with most yields (62% or 26/42) owing to HRF and CRR events. Whereas these were often non-ABO (minor antigen-targeting) antibodies (76% or 25/33) and followed reactions to red blood cell transfusions (RBC), the yields from complicated allergic reactions and "other" reactions were entirely due to passively acquired isoagglutinins (11/11). The former non-ABO antibodies were revealed by IAT (with no additional gains from elution studies), while ABO isoagglutinins were revealed by DAT alone (and type-specific eluates), and followed plasma (antibody-) containing products. IVIG-associated reactions exhibited the highest serologic yields (in 48% of cases, or in 70% of non-O type recipients), with 60% experiencing some degree of hemolysis.
Conclusion: A fifth of reactions were either over-tested or under-tested. Analysis of the performance and contextual yields of serologic tests revealed that certain products and presentations merit greater attention while others merit less. The IAT is a greater priority than the DAT in HRF and CRR following RBC, while the DAT alone is informative in isoagglutinin-risk cases, irrespective of presentation type, and with predictable eluate specificities. A re-evaluation of traditional serologic testing reflexes may reduce costs and allow re-investment in other more informative reaction-specific assays.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal